COVID-Tongue Was Just the Beginning — Say Hello to COVID-Mouth
Health Desk- Martian Smiles Lab
New Delhi, UPDATED June 07, 2025 07:12 pm
As new COVID variants like NB.1.8.1 and Nimbus re-emerge across parts of India, Europe, and the U.S. in 2025, it’s a stark reminder that the pandemic’s story isn’t over — especially when it comes to your mouth.
While the spotlight has long been on the virus’s respiratory effects, a growing number of long-COVID survivors are sounding the alarm on something often overlooked: persistent oral symptoms. From burning tongues and unexplained ulcers to dry mouth and taste loss, COVID-19 continues to leave a hidden imprint in the mouths of recovering patients.
In this article, we shine a light on these lesser-known effects — a constellation of symptoms now recognized as “COVID-Mouth.” Whether you’re a dental professional, a long-hauler, or simply curious, what follows is a timely wake-up call: because sometimes, your mouth speaks what your body can’t.
Beyond the Lungs: COVID’s Silent Assault on the Mouth
When COVID-19 first emerged, its most alarming symptoms — shortness of breath, fever, and lung inflammation — dominated headlines. But as our understanding of the virus has evolved, so too has our awareness of its more subtle, lingering effects. Among the most overlooked of these is the virus’s impact on the mouth.
What began as isolated reports of a “COVID tongue” has grown into a broader pattern of oral complications: burning sensations, persistent dry mouth, inflamed taste buds, sore throats, and strange discolorations or lesions on the tongue. These symptoms, once dismissed as unrelated or temporary, are now surfacing in more and more long COVID patients.
One user on Reddit described a striking experience — initially presenting with red spots and depapillation on the tongue, followed by chronic burning mouth, dry throat, and lingering chest congestion that persisted weeks after infection. “Anyone else have a similar problem?” they asked — a question now echoed by thousands across support forums and dental practices.
These firsthand accounts are forcing clinicians to rethink the oral manifestations of COVID. It’s no longer just about “COVID tongue.” We’re witnessing the emergence of a broader, more systemic oral syndrome — one that deserves its own name: COVID-Mouth.
What Is COVID-Mouth?
“COVID-Mouth” is an umbrella term coined by Dr. Bibhakar Ranjan to describe a range of oral health symptoms linked to COVID-19, observed both during the active phase of the infection and in cases of long COVID. These symptoms vary in severity and include:
- A swollen, patchy, or discolored tongue (often referred to as “COVID tongue”)
- Dry mouth (xerostomia)
- Mouth ulcers or blisters
- Burning sensations in the mouth
- Cracks at the corners of the lips (angular cheilitis)
- Bleeding or inflamed gums
- Loss or alteration of taste (dysgeusia)
These COVID-Mouth symptoms can appear in isolation or as a group, and may last for weeks or even months. While some patients experience only mild discomfort, others report significant pain or disruptions to daily life.
Why the Mouth?
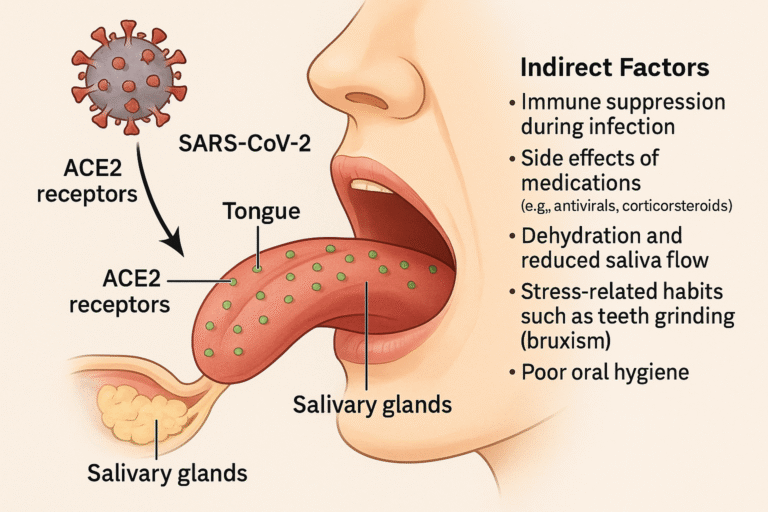
The mouth, often considered a window to our overall health, is rich in ACE2 receptors — the very receptors that SARS-CoV-2, the virus behind COVID-19, uses to enter human cells. These receptors are found in abundance on the tongue, the inner lining of the cheeks, and the salivary glands. This makes oral tissues a direct target for the virus.
In addition to direct viral invasion, several indirect factors contribute to oral symptoms:
- Immune suppression during infection
- Side effects of medications used during treatment (e.g., antivirals, corticosteroids)
- Dehydration and reduced saliva flow
- Stress-related habits such as teeth grinding (bruxism)
- Poor oral hygiene during illness or isolation
Clinical Observations from the Frontlines
During the height of the pandemic, Dr. Bibhakar Ranjan, then serving as a dental practitioner in Seychelles, began observing unusual oral complaints among post-COVID patients. Although many had already tested negative for the virus, they continued to report persistent symptoms such as dry mouth, altered taste sensations, and a burning feeling on the tongue.
Some were so severe they could not eat spicy or acidic foods without discomfort. In certain cases, He observed secondary fungal infections due to prolonged dryness or steroid use. As more and more of these cases appeared, it became clear that we weren’t just dealing with dental side effects — we were seeing the systemic effects of a virus that was rewriting how we understood oral health.
What the Research Says
New @NatureMedicine
— Eric Topol (@EricTopol) March 25, 2021
"The oral cavity is an important site for SARS-CoV-2 infection and implicate saliva as a potential route of SARS-CoV-2 transmission."https://t.co/UTfsc86XNP
Elegant work. Saliva from asymptomatic individuals transmitted covid ex vivo pic.twitter.com/G9SeSIoKSB
Studies from around the world are beginning to catch up. A 2022 review in the Journal of Dental Research found that up to 45% of moderate to severe COVID-19 patients reported oral symptoms. Another study published in Nature highlighted the detection of SARS-CoV-2 in saliva and oral mucosal tissue, emphasizing the importance of the oral cavity in both transmission and symptom manifestation. A growing number of studies are confirming that COVID-Mouth symptoms may be present even in mild cases.
Emerging technologies like AI-powered diagnostics and teledentistry platforms are also aiding in documenting and identifying patterns in post-COVID oral issues. Researchers are exploring how oral microbiome changes may contribute to long COVID symptoms, and whether saliva testing can serve as a reliable tool for early detection.
COVID-Mouth in the Long Haul
The American Academy of Otolaryngology posted information on its website saying that mounting anecdotal evidence indicates that lost or reduced sense of smell and loss of taste are significant symptoms associated with Covid-19 https://t.co/IhO03Id2Bt
— The New York Times (@nytimes) March 23, 2020
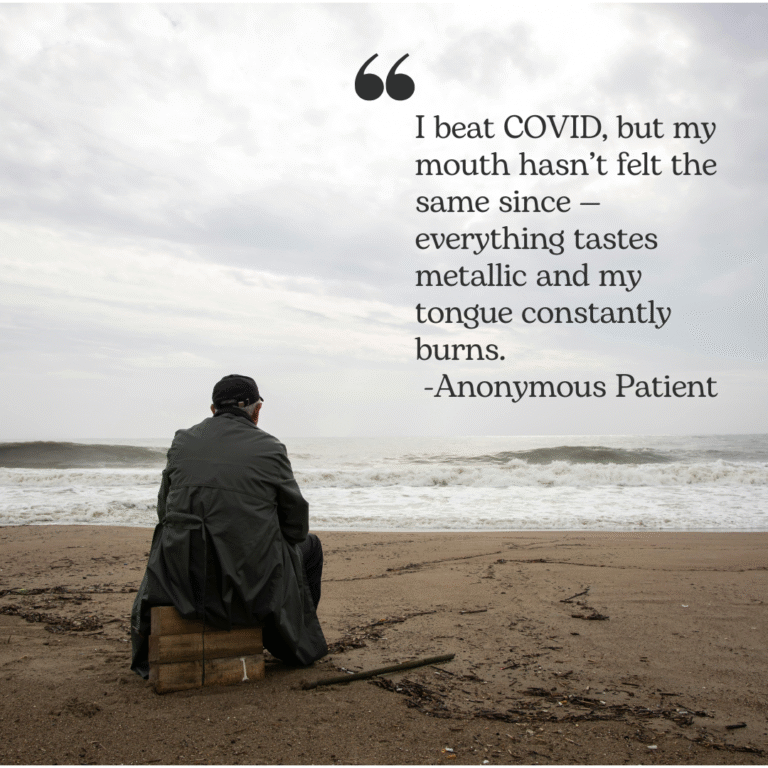
Even as the world opens up and vaccines reduce the risk of severe illness, long COVID continues to be a real concern. COVID-Mouth is now being studied as a component of long COVID, where patients report lingering oral discomfort, taste disturbances, or sensitivity for months post-infection. The link between chronic inflammation and oral symptoms is under investigation, with many suggesting that the oral cavity could serve as a marker for systemic recovery.
One real-world case involved a patient who continued to suffer from a burning mouth sensation and metallic taste for six months after recovering from COVID. No clear diagnosis could be given at the time, but the symptoms eventually subsided with a combination of nutritional support, topical treatments, and guided oral care.
Reframing Oral Health in the Post-COVID Era
I'm a physician with #LongCovid. Here's two cents.
— Zeest Khan, MD (@doctor_zeest) August 22, 2024
Please go to the dentist. The risk of missing an oral infection/cancer outweighs most anything else.
If you haven't seen endocarditis, or jaw necrosis, much less catastrophic facial pain from tooth decay, don't argue with me.
The emergence of COVID-Mouth underscores the importance of regular dental checkups and open communication with both dentists and doctors. Many people still don’t associate oral symptoms with systemic illnesses. It’s time we rethink that assumption.
Preventive oral care, hydration, a balanced diet, and early detection strategies can go a long way in mitigating the effects of COVID-Mouth. Dentists must be included in the long COVID recovery ecosystem, not just as caregivers for the teeth, but as frontline observers of larger systemic changes.
What You Can Do Now
If you or someone you know has had COVID-19 and is experiencing any of the symptoms listed above, consider these steps:
- Stay hydrated: Dry mouth worsens many of these symptoms.
- Resume oral hygiene: Brush twice daily, use alcohol-free mouthwash, and floss regularly.
- Avoid irritants: Spicy, acidic, and overly salty foods may trigger discomfort.
- Consult your dentist: Don’t ignore oral symptoms thinking they’re minor.
- Keep a journal: Track when symptoms appear and whether they improve over time.
The Bigger Picture

COVID-Tongue was just the tip of the iceberg. As new waves of COVID-19 quietly resurface in India, the United States, China, and several other countries, it’s clear the pandemic’s long-term effects are far from over. Amidst this renewed concern, oral health must become part of the broader conversation. Whether it’s a dry mouth that won’t go away or a tongue that feels like it’s on fire, your mouth might be trying to tell you something important about your recovery. Ignoring lingering COVID-Mouth symptoms may delay proper diagnosis or care.
So, the next time you look in the mirror and stick out your tongue, remember: COVID-Mouth is real — and it’s time we took it seriously.
Official Address
- Bonn, Germany
- Victoria, Mahe Island, Seychelles
- New Delhi, India.
- info@drbibhakarranjan.com
- +49 15560 936114
Copyright 2025 Dr Bibhakar Ranjan – All Rights Reserved
